Research gaps based on drowning timeline – Questions to be answered
OBJECTIVE
Provide a detailed description of research gaps and question examples along the drowning process using the DROWNING TIMELINE, including triggers, actions and consequent interventions, where a good level scientific evidence is still lacking. With this section we aim to raise important topics and provide powerful insights as a tool to prioritize all interventions needed considering the measurement of future cost/benefit ratios related to outcome in terms of public health, financial aspects, political scope and social impacts.
But please, have fun reading through this section and looking for the most appealing and interesting questions to be answered. We are positive that the number of gaps and questions to be made are enormously bigger than posted here, be stimulated to increase it.
IMPORTANT NOTES ABOUT THIS SECTION
• Each gap/question will be referred to include one or more reference to the drowning timeline.
• Let us know if you want to rephrase or include any other gap and/or question(s).
• Each raised question is not definitive, can be modified by the proponent researcher.
• Each GAP/question will be rated as VERY RELEVANT(****), RELEVANT(***), MEDIUM(**) or LOW(*) according to its impact on public health, financial aspects, political scope and social impacts (following the rating attributed by the members).
• We encourage all of you to indicate relevant literature to the topic (being it a gap or question). Please consider the highest scientific evidence level published (Oxford (UK) CEBM Levels of Evidence(LOE) in GAP section (insert the LOE besides the reference).
• We encourage all authors to share their projects/research in progress, making others aware of what’s being studied, facilitating the exchange of information and avoid duplication of efforts.
GRAPHIC
DROWNING TIMELINE TERMINOLOGY DESCRIPTION
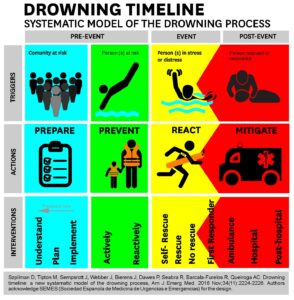
Phase: corresponds to a part in a series of related actions of the drowning timeline, before it starts, during the process and after it ends. In the current model there are 3 phases: pre-event, event and post-event.
Triggers: Anything that serves as a stimulus and initiates or precipitates an action. In this model we have identified “community at risk” as the trigger for preparation; “person(s) at risk” as the trigger for prevention; “person(s) in stress/distress as the trigger for reaction; and “person being rescued or rescued” as the trigger for mitigation.
Action: Any measure taken during any phase of the drowning timeline will necessarily fall in one of 4 categories of action: prepare, prevent, react or mitigate that will be activated by specific triggers and will lead to specific interventions.
Intervention: Is any measure taken during a specific category of action that will have influence on what happens, modifying or hindering the impact of a drowning event.
Pre-event: The pre-event is the phase before the drowning process starts and comprises two actions (preparation and prevention) that were triggered either by a community at risk (preparation) or a person or group at risk (prevention).
Event: The event phase encompasses any action taken in the water triggered by a person in stress or distress, while the drowning process is taking place. Possible actions are: self-rescue, rescue, or no rescue. If the rescue is being performed by a first responder, being it a layperson or a professional, some mitigation interventions might take place while the victim is still in the water, such as first in-water efforts to provide life-support.
Post-event: The post-event phase is only composed of mitigation actions – those that will make the impact of the drowning less severe, harmful, or painful. It starts after extrication from the water has ended and extends until all the health care ceases, such as ambulance attendance, hospital and post-hospital care.
INTRODUCTION
The triggers are simply the identification of a community at a risk of drowning for any reason. Actions are directed at communities at risk, taken before an incident aimed at improving effectiveness of Prevent, React and Mitigate actions. The rationale for the separation of this concept in the timeline is of major importance. Many of the interventions in the “preparation” category have been mistakenly taught as a type of preventative interventions, when they are more about being “prepared to react or to mitigate” the injuries/death rather than actually preventing the incident (the contact between human and the trauma agent) from happening.
Preparation to prevent consists of education in its different forms usually away from aquatic setting, e.g. educational videos, billboards, school activities and others.
Preparation to react consists of learning how to react to danger situation to yourself or others in an aquatic setting, e.g. learn how to swim, recognizing a potential drowning victim, and/or rescue techniques.
Preparation to mitigate consists of training in and outside an aquatic setting, including learning drowning and CPR protocols. All forms of preparation can be taught both to the general public to professionals, but the contents and responsibilities might differ.
For each category have 3 interventions: Understand the problem, Plan the best strategy to fight the problem, and Implement the plan and verify its effectiveness.
PREPARE IN GENERAL (INCLUDING MORE THAN ONE SINGLE ACTION)
G: Knowing the whole drowning problem at local, regional and national (****)
Q: What and where are the sources to collect the figures on drowning?
Q: What data to collect on drowning?
Q: Definition and terminology on drowning – Is there any consensus at all?
REF1: World Health Organization. Global Report on Drowning. World Health Publications; 2015. (LOE4)
REF2: Van Beeck EF, Branche CM, Szpilman D, Modell JH, Bierens JJLM. A new definition of drowning: towards documentation and prevention of a global public health problem. Bull World Health Organ 2005;83:853–6.(LOE5)
REF3: Idris AH, Berg RA, Bierens J, Bossaert L, Branche CM, Gabrielli A, et al. Recommended guidelines for uniform reporting of data from drowning 2003 (LOE5)
REF4: Szpilman David, Tipton Mike, Sempsrott Justin, Webber Jonathon, Bierens Joost, Dawes Peter, Seabra Rui, Barcala-Furelos Roberto, Queiroga Ana Catarina, Drowning timeline: a new systematic model of the drowning process, American Journal of Emergency Medicine (2016), doi: 10.1016/j.ajem.2016.07.063. Submitted June 1, and accepted at July 28, 2016.(LOE5)
G: Effectiveness of lifesaving service (***)
Q: What is the best relation between prevention X rescue X mitigation actions?
Q: What is the cost and the effectiveness of each action of the drowning timeline for a lifesaving service?
REF1: Szpilman David, Tipton Mike, Sempsrott Justin, Webber Jonathon, Bierens Joost, Dawes Peter, Seabra Rui, Barcala-Furelos Roberto, Queiroga Ana Catarina, Drowning timeline: a new systematic model of the drowning process, American Journal of Emergency Medicine (2016), doi: 10.1016/j.ajem.2016.07.063. Submitted June 1, and accepted at July 28, 2016.(LOE5)
G: Lifesaving sport (*)
Q: What are the return values from lifesaving competition for the burden of drowning?
Q: Are we using the lifesaving tool for the best to reduce the burden of drowning?
Q: Lifesaving sport – Does it fit as a preventive tool?
REF1:
G: Anatomopathology (usually post-mortem) (***)
Q: What is the strongest evidence to drowning diagnostic?
Q: How to differentiate a primary from a secondary (precipitant disease) drowning?
REF1:
PREPARE TO PREVENT
G: Education on active prevention action(****)
Q: What has more impact, visual, written, or audio estimulus or a combo?
Q: What color and signs are more usefull to call for people’s attention?
REF1:
G: Education on reactive prevention action(****)
Q: How many tips are needed to spot/ recognize a bather/swimmer in iminent danger?
Q: What is the most impacting message to convice a bather/swimmer that he is at iminent risk?
Q: What are the pitfalls of beach surveillance?
REF1:
PREPARE TO REACT
G: Education on self-rescue(***)
Q: What are the basic swimming skills for each aquatic environment?
Q: Difficulty in the water: How to avoid getting into distress?
REF1:
G: Education on rescue(***)
Q: What is the safest way to help without becomming a second vctim?
Q: What is the best lifesaving equipment on the surf beaches?
Q: How many decisions does a lifeguard have to make on a single rescue?
Q: How to decide who to pick first in a multiple victim scenario?
Q: What is the rate between the number of lifeguards and population at different aquatic scenarios?
Q: What would be the most appropriate lifeguard tower for each particular scenario?
REF1:
PREPARE TO MITIGATE
G: In-water mitigation education(**)
Q: Is the in-water education to lay public adequate?
Q: What’s the best way to teach in-water mitigation for lifeguards?
Q: What are the basic and advanced procedures to teach for in-water moment?
REF1:
G: Pre-hospital out-water mitigation(**)
Q: What maneuvers to teach regarding transportation of the patient from water to a dry place?
Q: What’s the best ratio students per manikin for effective learning and training of CPR?
Q: Advanced airways management on drowning victims: laryngeal mask vs oro tracheal tube?
REF1:
G: Education at Emergency room(**)
Q: What procedures to teach to ER staff regarding drowning victims?
Q: What are the difficulties on advanced management of the airways on drowning victims?
Q: How importance is to teach the drowning chain to health professionals?
Q: What would be the best way to teach the severity drowning classification?
REF1:
G: Education at Hospital attendance(**)
Q: What are the drowning basics skills to teach health professionals at the ER?
Q: How to calculate prognostic factor on drowning survival?
Q: What are the brain protective measures on post-CPR drowning?
Q: How long to keep the patient on artifical ventilation?
Q: Is the knowledge of the microorganism in the water where drowning occurred any good to decide on which antibiotic to use?
REF1:
G: Education for the post-hospital(*)
Q: What are and how the psychological effects of drowning affect a victim throughout his life?
Q: How to reduce the psychological effect of a drowning episode?
Q: What are the treatable vs untreatable sequels from a drowning episode?
Q: Is there a need to return and seek medical consultant after all?
REF1:
Including any actions directed to risky environments and users, and taken before an incident aimed at stopping the drowning event from occurring. Is triggered by a person(s) at risk and has been mistaken described as one single category of intervention, however, this we’ve identified two different categories of prevention entailing distinct types of interventions:
Active prevention: actions directed to a specific area or detection of risky behaviours at the scene such as proactively placing warning signage to sign a rip current or identifying and signage environment hazards or behaviours.
Reactive prevention, actions directed at specific individuals or groups to stop an imminent danger such as a lifeguard whistling to a bather who is at imminent risk and directing them to safety or by simply removing bather or group from the dangerous situation before the event of drowning starts (risky activities).
Gaps (G) and examples of possible raised Questions (Q)
ACTIVE
G: Cost of active prevention actions taken versus benefits.(****)
Q: Which active preventive action is more cost-effective for pool safety?
G: Major active actions VS minor ones.(****)
Q: Warning signage is more effective than prohibiting access to risky areas?
G: Active prevention actions on areas of great risk of tsunamis.(**)
Q: What are the measures to keep population safe against tsunamis?
G: Active prevention actions on river safety(****)
Q: How to impact with preventive measures the so scattered river population?
G: Active prevention action affecting drowning burden(****)
Q: How is the identification of reducing of drowning figures related to active prevention?
Q: What is the first step in preventing drowning? Does it start with pool fences, public education, swim lessons, or some other intervention?
REF1:
REACTIVE
G: Lifeguard cost of active VS reactive prevention actions.(****)
Q: Are lifeguarding services (an active and reactive preventive staff) more cost-effective than population educational well-designed and implemented programs (preparation)?
G: Too late VS too early lifeguard whistling to a bather who is at imminent risk.(****)
Q: What are the pitfalls for a lifeguard when whistling too early or too late to a bather/swimmer in danger?
G: Reactive prevention actions on areas of great risk of tsunamis.(**)
Q: Are the warning systems effective?
G: Reactive prevention actions on a flood(***)
Q: How are the safety procedures in a flood while in the car?
REF1:
Any action taken during the water stage is regarded as the event phase, which coincides with reaction in the timeline. Reaction initiated by a stressful condition, when a person feels at risk of drowning, followed or not by a distress situation when the ability to rationally cope with the stressful condition is overwhelmed. Actions directed at a person (or group) in stress or distress and taken after an incident while in water aimed at interrupting the progress of drowning once it started. Reaction will only stop with the extrication from the water/danger
Self-rescue occurs when the person is able to get out of the difficult situation without external assistance, usually reaching only stress.
Rescue occurs when the person is assisted by someone else (can be a relative, a friend, a lifeguard).
No-rescue is when help is needed but not provided.
Gaps (G) and examples of possible raised Questions (Q)
SELF-RESCUE
G: Self-rescue
Q: What mechanisms a self-rescued victim used to escape?
Q: Is it possible to reduce the heat loss during long recues?
Q: How many victims in trouble wave and/or shout for help?
Q: Is it possible to self-rescue while in distress?
RESCUE
G: Rescue
Q: In a common lifeguarding service day, what is the number/ratio of rescues made withouth getting in water?
Q: From all rescues done, how many drowning victim were in cardiac arrest?
Q: Using the start triage system on rescues what are the odds for each drowning grade?
Q: What is the most usefull floatation equipment for a daily use?
NO-RESCUE
G: No-rescue
Q: What are we missing about the vicitms not rescued?
Usually starts when the victim is still in contact with the ‘trauma aggressor’ and before extrication from the water has ended. Start with actions directed at a specific person, or group, taken while performing the rescue or immediately after the rescue aimed at reducing the impact of the injury on the victim(s). Casualty assessment during the event phase induces in-water mitigation actions. Mitigation actions in the post-event phase are initiated only after extrication from immediate danger has ended. The overlapping section between reaction and mitigation actions represents the intersection of the two actions. This occurs when the victim is being rescued and the rescuer is also applying mitigating interventions to reduce the impact of the drowning process before removing the victim from the water. During the event mitigating interventions are usually performed by professionals, such as lifeguards or first responders and may include: opening the airway while rescue is taking place; a first responder performing in-water ventilations; providing oxygen using a facemask while extricating an individual from a water disaster like a flood, but still in a boat and in danger. During the post-event phase includes all interventions related to provision of health care and can be categorized as: local (ambulance), at hospital; and post-hospital interventions and may include: a drowning victim being assisted in a critical situation at the beach; specific health care provided during transportation to a ER and hospitalization; home care rehabilitation (after release from hospital) which can include physical and psychological assistance.
Gaps (G) and examples of possible raised Questions (Q)
IN-RESCUE MITIGATION
G: In-rescue mitigation
Q: In which cases in-water mitigation is needed/useful?
Q: What is the best lifeguard equipment to help conduct in-water mitigation procedures?
Q: When to proceed and not on doing in-water mitigation?
PRE-HOSPITAL MITIGATION
G: Pre-hospital out-water mitigation
Q: What is the safest way to transport the patient from water to a dry place?
Q: What are essential basic and advanced medical equipment to have for drowning?
Q: Drowning approach: Victim to the hospital or hospital to the victim?
Q: Cervical immobilization: When is it really indicated?
EMERGENCY ROOM MITIGATION
G: Emergency room
Q: How is the triage by severity of drowning arriving at ER?
Q: What complementary exams to ask for a drowning patient based on severity?
Q: Is there any refusing to resuscitate at the ER?
HOSPITAL MITIGATION
G: Hospital attendance
Q: Whose drowning patients to send to intensive care units?
Q: Hypothermia is protective in which drowning patients?
Q: Prognostic need to be based on drowning severity?
POST-HOSPITAL MITIGATION
G: Post-hospital
Q: How many need psychological care?
Q: How a drowning affects a victim in the next 20 years of their lifes ?
Q: How many need physical reabilitation care?
WHY SO MANY GAPS IN DROWNIG RESEARCH?
For people between the ages of 5 and 44 years, injuries are one of the top three causes of death [1], representing 10% of the world’s deaths [2]. Injuries are the consequence of trauma resulting from any exposure to energy, mechanical, thermal, electrical, chemical or radiation, that overcome the body’s defences and cause damage [3]. Injuries can be physical or psychological, temporary or permanent, intentional or unintentional, and can vary from mild to severe. Drowning is one of the major causes of trauma [4], killing 372,000 people per year worldwide, most of which is preventable.
Since some cases of fatal drowning are not classified as such according to the codes of the International Classification of Disease, this number underestimates the real figures, even for high-income countries [5], as these numbers do not include drownings that occur as a result of floods, tsunamis, and boating accidents [6] Furthermore, an estimated 90% of all drowning deaths occur in low- and middle- income countries, which contributes to a major under-reporting. Limited data are available because many are pronounced dead on scene and never make it to a hospital therefore are not formally recorded in death or trauma registries [4]. Drowning deaths at the hospital are, in some cases, misjudged and drowning is not coded as the primary cause, so a significant number of incidents are missing the ICD code that would allow for a proper analysis of the drowning problem. Additionally, to date, the burden of drowning has primarily been measured using information from resuscitation attempts [7] and hospitalizations, which excludes the majority of the problem: non-fatal drowning cases. Therefore, drowning burden is left with incomplete datasets and a greatly underestimated.
The first steps in addressing the under-reporting of drowning have recently been taken through consensus building meetings among drowning experts [4,7], with the focus to date being the creation of guidelines and extensively advocating for uniform reporting of data from drowning. However, improved, standardized, and integrated data collection systems on drowning are still needed. Definitions, terminology and data collected by local, national, and international agencies is not uniform, as evidenced by peer-reviewed literature, national drowning reports and media releases [8,9], where, for example, authors still commonly define as preventive activities interventions that do not prevent the drowning process but instead aim to reduce its negative impact on the victim. Additionally, prevention, rescue and life-support services are typically provided by distinct agencies, which report their own data without follow-up or linkage with downstream care.
Underreporting contributes significantly to misunderstanding of the process of drowning and compounds the difficulties of data comparison. Estimates show that underreporting can comprise as much as 94% of all drowning events [6]. Filling these scientific gaps requires building a worldwide consensus on definitions, terminology and clearly defining what data to collect on fatal and non-fatal drowning.
Addressing drowning as a traumatic event and utilizing the drowning timeline can bridge the gap in defining and understanding the whole drowning process and allow researchers to to set what is scientific evidence-based on each phase and actions and find questions need to, but not been answered yet.
As with other types of trauma, the lack of clear-cut distinctions between pre-event, event and post-event, as well as between triggers, actions and interventions, hampers the systematic collection of drowning-related data. This, in turn, has severe impacts on the quality of the estimates of the global burden of drowning, and consequently on the effectiveness of drowning prevention strategies.
REFERENCES
[1] Injuries and Violence in Europe. World Health Organization; 2010.
[2] World Health Statistics 2015. Geneva: World Health Organization; 2015.
[3] Baker SP, Li G, Ginsburg MJ, O’Neill B. The Injury Fact Book. Second Edition. 1992.
[4] World Health Organization. Global Report on Drowning. World Health Publications; 2015.
[5] Lu T-H, Lunetta P, Walker S. Quality of cause-of-death reporting using ICD-10 drowning codes: a descriptive study of 69 countries. BMC Med Res Methodol 2010;10:30. doi:10.1186/1471-2288-10-30.
[6] Szpilman D, Bierens JJLM, Handley AJ, Orlowski JP. Drowning. N Engl J Med 2012;366:2102–10. doi:10.1056/NEJMra1013317.
[7] Idris AH, Berg RA, Bierens J, Bossaert L, Branche CM, Gabrielli A, et al. Recommended guidelines for uniform reporting of data from drowning 2003.
[8] Papa L, Hoelle R, Idris A. Systematic review of definitions for drowning incidents. Resuscitation 2005;65:255–64. doi:10.1016/j.resuscitation.2004.11.030.
[9] Sempsrott J, Slattery D, Schmidt A, Penalosa B, Crittle T. Systematic Review of Non-Utstein Style Drowning Terms. Annals of Emergency Medicine 2011;58:S321. doi:10.1016/j.annemergmed.2011.06.456.
[10] Haddon W. The changing approach to the epidemiology, prevention, and amelioration of trauma: the transition to approaches etiologically rather than descriptively based. 1968. vol. 5. BMJ Publishing Group Ltd; 1999.
[11] Federation ILS. Drowning Prevention Strategies. 2015.
[12] Peden M, Oyegbite K, Ozanne-Smith J, Hyder AA, Branche C, Rahman AF, et al. World Report on Child Injury Prevention. Geneva: World Health Organization; 2008.
[13] Van Beeck EF, Branche CM, Szpilman D, Modell JH, Bierens JJLM. A new definition of drowning: towards documentation and prevention of a global public health problem. Bull World Health Organ 2005;83:853–6.
[14] Brenner RA, Saluja G, Smith GS. Swimming lessons, swimming ability, and the risk of drowning. Injury Control and Safety Promotion 2003;10:211–5. doi:10.1076/icsp.10.4.211.16775.
[15] Tipton M, Golden F. Essentials of Sea Survival. Human Kinetics; 2002.
[16] Wallis BA, Watt K, Franklin RC, Taylor M, Nixon JW, Kimble RM. Interventions associated with drowning prevention in children and adolescents: systematic literature review. Inj Prev 2015;21:195–204. doi:10.1136/injuryprev-2014-041216.
[17] Leavy JE, Crawford G, Portsmouth L, Jancey J, Leaversuch F, Nimmo L, et al. Recreational Drowning Prevention Interventions for Adults, 1990–2012: A Review. J Community Health 2015:1–11. doi:10.1007/s10900-015-9991-6.
[18] Fink G, editor. Stress Science. Oxford: Academic Press; 2010.
[19] Szpilman D, Webber J, Quan L, Bierens J, Morizot-Leite L, Langendorfer SJ, et al. Creating a Drowning Chain of Survival. Resuscitation 2014. doi:10.1016/j.resuscitation.2014.05.034.
[20] Venema AM, Groothoff JW, Bierens JJLM. The role of bystanders during rescue and resuscitation of drowning victims. Resuscitation 2010;81:434–9. doi:10.1016/j.resuscitation.2010.01.005.
Oxford (UK) CEBM Levels of Evidence
1a: Systematic reviews (with homogeneity) of randomized controlled trials
1b: Individual randomized controlled trials (with narrow confidence interval)
1c: All or none randomized controlled trials
2a: Systematic reviews (with homogeneity) of cohort studies
2b: Individual cohort study or low quality randomized controlled trials (e.g. <80% follow-up)
2c: “Outcomes” Research; ecological studies
3a: Systematic review (with homogeneity) of case-control studies
3b: Individual case-control study
4: Case series (and poor quality cohort and case-control studies)
5: Expert opinion without explicit critical appraisal, or based on physiology, bench research or “first principles”